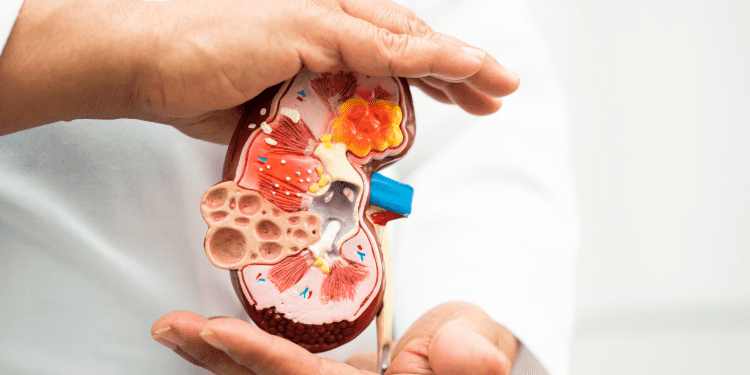
Glomerulonephritis (GN) is a term that refers to a group of kidney diseases characterized by inflammation of the glomeruli, which are the small filtering units in the kidneys responsible for removing waste and excess fluids from the blood. The inflammation typically affects both kidneys simultaneously. Glomerulonephritis can be acute, with a sudden onset, or chronic, developing over a more extended period. It can be a primary condition or secondary to other underlying diseases or infections
General Definition of Glomerulonephritis:
Glomerulonephritis is a kidney condition marked by inflammation of the glomeruli, affecting their ability to filter blood and leading to symptoms such as hematuria, proteinuria, edema, and hypertension. It can be acute or chronic, with causes ranging from infections to autoimmune disorders.
Types of Glomerulonephritis:
There are Two Types of Glomerulonephritis Acute and Chronic Based on Their onset and progression due to distinct underlying mechanisms and pathophysiological processes.
1. Acute Glomerulonephritis:
Acute Glomerulonephritis is a sudden inflammation of the glomeruli, the kidney’s filtration units, typically triggered by infections, especially streptococcal infections. It manifests with symptoms like hematuria, proteinuria, and reduced glomerular filtration rate, and may lead to fluid retention and hypertension.
Etiology :
The primary etiology of acute glomerulonephritis (AGN) is often related to a preceding infection, particularly with certain strains of the bacteria Streptococcus. The most common form is post-streptococcal glomerulonephritis. Other infectious agents and non-infectious causes can also contribute
1. Streptococcal Infections :
- Group A Streptococcus (GAS): AGN frequently follows infections, particularly streptococcal throat infections (such as strep throat) or skin infections (like impetigo) caused by Group A Streptococcus.
2. Other Infections:
- Bacterial Infections: In addition to streptococcal infections, other bacterial infections such as staphylococcal, pneumococcal, and others can trigger Acute Glomerulonephritis.
- Viral Infections: Certain viral infections, including hepatitis B, hepatitis C, and HIV, can be associated with Acute Glomerulonephritis.
3. Non-Infectious Causes:
- Autoimmune Diseases: Systemic autoimmune diseases, like lupus erythematosus, may lead to Acute Glomerulonephritis due to immune complex deposition in the glomeruli.
- IgA Nephropathy: An immune-related condition where abnormal IgA immune complexes are deposited in the glomeruli.
4. Environmental Factors:
- Environmental Exposures: Some environmental factors, such as exposure to certain toxins or medications, may contribute to the development of AGN.
5. Genetic Predisposition:
- Genetic Factors: There may be a genetic predisposition, as some individuals may be more susceptible to developing Acute Glomerulonephritis based on their genetic makeup.
Pathogenesis:
- The common thread in AGN is the formation of immune complexes, which are aggregates of antibodies and antigens. These immune complexes can deposit in the glomeruli, leading to inflammation.
- The immune system’s response to infections or autoimmune processes results in the production of antibodies and the activation of the complement system.
- The deposited immune complexes can trigger an inflammatory response in the glomeruli, causing damage to the glomerular basement membrane and impairing the kidney’s normal filtration function.
Pathophysiology:
The pathophysiology of acute glomerulonephritis (AGN) involves a complex interplay of immune responses, inflammation, and damage to the glomeruli, the filtering units of the kidneys
1. Immune Complex Formation:
- AGN often begins with an initial infection, commonly caused by Streptococcus bacteria. During the infection, the immune system produces antibodies in response to the invading microorganisms.
- Immune complexes form when antibodies bind to antigens, typically from the infecting microorganisms. These complexes circulate in the bloodstream.
2. Deposition of Immune Complexes in Glomeruli:
- The immune complexes can deposit in the glomeruli, particularly within the glomerular capillaries and the mesangium (the supportive tissue between glomerular capillaries).
- This deposition triggers an inflammatory response within the kidney.
3. Activation of the Complement System:
- The immune complexes activate the complement system, a cascade of proteins that participate in the immune response.
- Complement activation results in the release of inflammatory mediators, attracting immune cells to the site of deposition in the glomeruli.
4. Inflammation and Injury:
- Inflammatory cells, such as neutrophils and macrophages, migrate to the glomeruli in response to the immune complexes.
- These cells release enzymes and cytokines, contributing to inflammation and causing damage to the glomerular basement membrane.
5. Increased Permeability of Glomerular Membrane:
- Inflammation and damage to the glomerular basement membrane lead to increased permeability.
- The increased permeability allows the leakage of red blood cells and proteins into the urine, leading to hematuria (blood in urine) and proteinuria (protein in urine).
6. Decreased Glomerular Filtration Rate (GFR):
- The inflammatory processes impair the normal functioning of the glomeruli, resulting in a decreased glomerular filtration rate (GFR).
- Reduced GFR contributes to fluid retention, hypertension, and other systemic symptoms
7. Clinical Manifestations:
- Patients with AGN may present with symptoms such as hematuria, proteinuria, oliguria (reduced urine output), edema (fluid retention), and hypertension.
- Systemic symptoms, including fever and malaise, may also occur, especially if AGN is secondary to an infection.
2. Chronic Glomerulonephritis:
Chronic glomerulonephritis (CGN) is a progressive and long-term condition characterized by the gradual deterioration of the glomeruli, the filtering units of the kidneys. Over time, repeated episodes of glomerular inflammation lead to scarring and fibrosis, resulting in a decline in renal function. CGN can be asymptomatic in the early stages, with symptoms becoming more apparent as the disease progresses. It often culminates in chronic kidney disease (CKD) and may ultimately necessitate renal replacement therapy, such as dialysis or kidney transplantation.
interstitium are hyalinised and thickened while the interstitium shows fine fibrosis and a few chronic inflammatory cells
Etiology:
The etiology of chronic glomerulonephritis can be diverse, and it may arise from various causes, including:
- Recurrent Acute Glomerulonephritis (AGN): Persistent or recurrent episodes of acute glomerulonephritis contribute to the chronic inflammatory processes and scarring.
- Systemic Diseases and Autoimmune Conditions: Chronic glomerulonephritis can be associated with autoimmune diseases like lupus erythematosus, as well as systemic conditions like diabetes mellitus.
- Hypertension: Prolonged, uncontrolled hypertension can lead to damage to the small blood vessels in the kidneys, contributing to chronic glomerular injury.
- Infections: Some chronic infections, such as chronic pyelonephritis, may result in persistent inflammation and damage to the glomeruli.
- Genetic Factors: There may be a genetic predisposition, with certain individuals being more susceptible to developing chronic glomerulonephritis.
Pathophysiology:
1. Progressive Glomerular Damage:
- Chronic glomerulonephritis is characterized by a persistent and gradual deterioration of the glomeruli, involving inflammatory processes and scarring.
- Over time, immune complex deposition repeated acute glomerular injuries, and prolonged inflammation contribute to the progressive damage of the glomerular architecture.
2. Reduced Nephron Number:
- The chronic inflammatory processes lead to the formation of scar tissue within the glomeruli, resulting in a decline in the number of functional nephrons.
- Nephron loss is a key feature of chronic glomerulonephritis, and the reduction in nephron number contributes to the decline in renal function and the progression of kidney disease.
3. Hypertension and Edema:
- As glomerular damage and nephron loss progress, the kidneys struggle to regulate blood pressure and fluid balance effectively.
- Hypertension ensues as a result of the kidneys’ reduced ability to excrete sodium and water. Edema, or fluid retention, occurs due to impaired filtration and increased fluid accumulation in the tissues.
- Hypertension and edema are significant clinical manifestations of advanced chronic glomerulonephritis and contribute to the overall morbidity associated with the condition.