Table of Contents
Introduction to Pathology Study Techniques
Pathology, the study of diseases, relies on a spectrum of techniques to examine tissues, cells, and biological samples. From traditional microscopy to cutting-edge molecular methods, these techniques aid in diagnosis, understanding disease mechanisms, and guiding treatment.
In this article, we have shared short notes about the topic and we explore classical and modern techniques used in clinical practice and research. Understanding these methods is crucial for healthcare professionals and researchers, as they underpin accurate diagnoses and advancements in medical knowledge. Let’s delve into the diverse tools that drive progress in pathology.
AUTOPSY PATHOLOGY
Introduction
Autopsy pathology is a branch of pathology that involves the examination of a body after death to determine the cause and manner of death, as well as to identify any diseases or injuries present. This examination is typically performed by a forensic pathologist, who is a medical doctor specializing in investigating the causes of sudden, unexpected, or suspicious deaths.
Historical Roots
- Autopsy pathology has its origins in the autopsy room, where early pioneers like G.B. Morgagni and T.H.A. Laennec embarked on the journey of understanding diseases.
- Their efforts laid the groundwork for clinicopathologic correlation (CPC), bridging the gap between clinical observations and postmortem findings.
Methods of Autopsy
- Block Extraction: This method involves the careful removal of abdominal and thoracic organs as a single unit, allowing for comprehensive examination.
- In Situ Dissection: Alternatively, organs can be dissected one by one in their original positions, facilitating a detailed exploration of individual structures.
Purpose and Significance:
- Quality Assurance of Patient Care:
- Autopsies serve as a vital tool for confirming the cause of death, establishing final diagnoses, and evaluating the effectiveness of treatments.
- Educational Value:
- They provide invaluable learning opportunities by identifying conditions that may have been missed clinically and discovering novel diseases.
- Autopsies contribute to our understanding of disease demographics, epidemiology, and the natural history of various conditions.
- Moreover, they offer essential educational experiences for students and pathology staff, fostering a deeper understanding of disease processes.
Challenges and Declining Rates:
- Despite their importance, autopsy rates have declined globally due to several factors.
- Advances in imaging technologies, such as CT and MRI, have provided physicians with higher diagnostic confidence, potentially reducing the perceived need for autopsies.
- Furthermore, concerns about legal liabilities have made some physicians wary of performing autopsies.
SURGICAL PATHOLOGY
Historical Roots:
- Surgical pathology, also known as histopathology or anatomic pathology, traces its origins back to the examination of tissues obtained during autopsies.
- Initially, surgeons relied solely on visible changes (gross findings) in tissues, discarding them afterward. However, advancements led to the development of diagnostic surgical pathology, focusing on microscopic examination of tissues.
Scope and Specializations:
- Surgical pathology has evolved into various subspecialties like nephropathology, neuropathology, and dermatopathology, each concentrating on specific organs or diseases.
- These subspecialties allow for detailed analysis and expertise in diagnosing various conditions.
Step-by-Step Protocol:
- Request Forms:
- Clinicians provide detailed patient information on request forms, including medical history, clinical findings, and previous tests.
- Tissue Accession:
- Laboratory staff match patient IDs on request forms with specimen containers. Tissues undergo different processing methods like fixation, freezing, or microwave fixation.
- Gross Room:
- Gross examination involves careful cutting and description of tissues. Proper handling and documentation prevent errors and ensure accurate diagnoses.
- Histopathology Laboratory:
- Tissues are processed using automated techniques for embedding and sectioning. Special procedures like frozen sectioning allow for rapid diagnosis during surgery.
- Staining and Microscopy:
- Tissue sections are stained using routine stains like hematoxylin and eosin (H&E) or special stains. Microscopic examination helps identify cellular abnormalities and make diagnoses.
- Surgical Pathology Report:
- Pathologists issue detailed reports containing patient history, gross and microscopic findings, and a diagnosis. Quality control measures ensure report accuracy.
- Quality Control:
- Regular monitoring and external quality control programs maintain diagnostic standards and reliability.
- Legal Considerations:
- Pathologists must report findings accurately, especially in complex cases. Internal and external consultations may be needed to minimize legal risks.
SPECIAL STAINS (HISTOCHEMISTRY)
Introduction
While hematoxylin and eosin (H&E) staining is the go-to method for diagnosing most surgical specimens, special circumstances may require the use of additional stains, known as histochemical stains. These stains help pathologists highlight specific substances or cellular components crucial for confirming various aspects of disease etiology, histogenesis, or pathogenesis.
Principles of Special Stains:
- Special stains work based on physical, chemical, or differential solubility properties with tissues.
- These stains provide selective coloration of specific cellular components or substances, aiding in their visualization under the microscope.
Commonly Used Special Stains:
- Amyloid Stains: Used to detect amyloid deposits in tissues, indicating certain types of diseases like amyloidosis.
- Carbohydrate Stains: Highlight the presence of carbohydrates in tissues, important for identifying glycogen storage diseases and other carbohydrate-related disorders.
- Lipid Stains: Staining methods for lipids are employed to visualize lipid-rich structures like fat cells or to detect abnormalities in lipid metabolism.
- Protein Stains: These stains help identify specific proteins or protein aggregates within tissues, aiding in the diagnosis of protein-related diseases.
- Nucleic Acid Stains: Used to visualize nucleic acids, essential for detecting abnormalities in DNA or RNA content within cells.
- Connective Tissue Stains: Highlight the presence of collagen and other components of connective tissue, aiding in the diagnosis of connective tissue disorders.
- Microorganism Stains: Employed to detect the presence of microorganisms such as bacteria, fungi, or parasites within tissues, crucial for diagnosing infectious diseases.
- Neural Tissue Stains: Used to visualize neural components like nerve fibers or cell bodies, aiding in the diagnosis of neurodegenerative disorders.
- Pigment Stains: Highlight the presence of pigments such as melanin or hemosiderin in tissues, important for diagnosing pigment-related disorders.
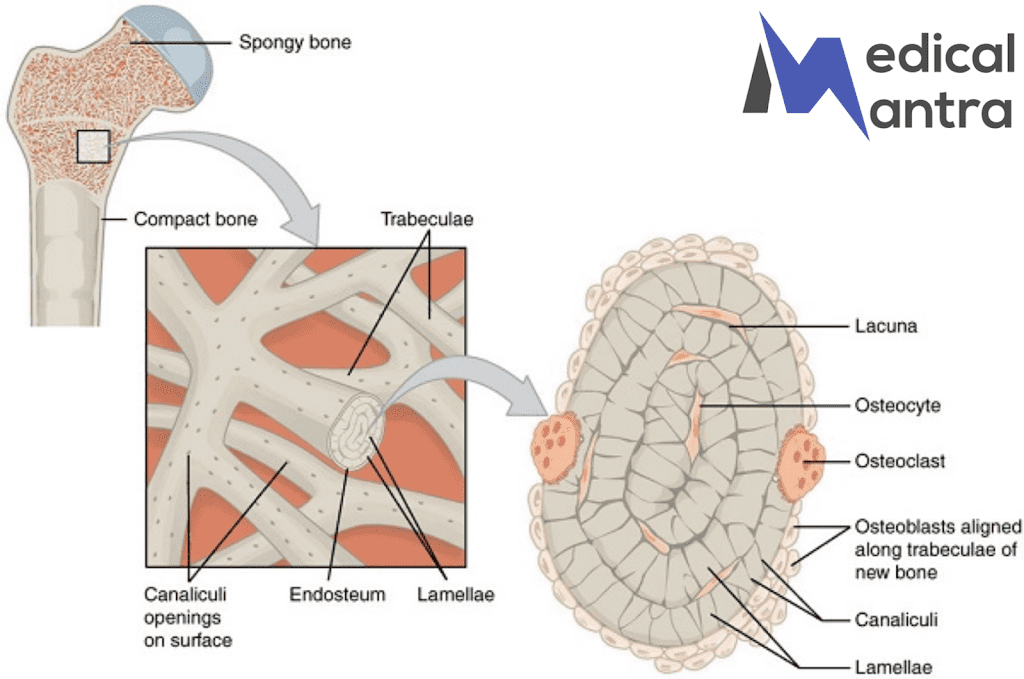
- Mineral Stains: These stains are utilized to detect mineral deposits within tissues, aiding in the diagnosis of metabolic bone diseases or mineralization disorders.
ENZYME HISTOCHEMISTRY
Introduction
Enzyme histochemical techniques are used to visualize specific enzymes within tissues, providing insights into cellular activity and function. While these techniques have historically been valuable in diagnostic pathology, their usage has declined due to limitations such as the requirement for fresh tissues and the advent of more advanced methodologies like immunohistochemistry and molecular pathology.
Principles and Applications:
- Requirement for Fresh Tissues: Enzyme histochemistry necessitates the use of fresh tissues for cryostat sectioning as enzymes degrade rapidly in formalin-fixed or paraffin-embedded tissues.
- Limited Diagnostic Applications: Despite their historical significance, enzyme histochemical techniques have limited diagnostic applications today. This is primarily due to the need for fresh tissues, the complexity of the techniques, and the lack of specificity in many cases.
Common Applications:
- Demonstration of Muscle-Related Enzymes (ATPase): Used in diagnosing myopathies by visualizing ATPase activity in muscle tissues.
- Acetylcholinesterase Staining: Helpful in diagnosing Hirschsprung’s disease by identifying the absence of acetylcholinesterase activity in affected tissues.
- Chloroacetate Esterase Staining: Used to identify myeloid cells and mast cells in various pathological conditions.
- DOPA Reaction: Detects tyrosinase activity in melanocytes, aiding in the diagnosis of melanocytic lesions.
- Viability of Cardiac Muscle: Endogenous dehydrogenase activity, assessed using nitroblue tetrazolium (NBT), indicates the viability of cardiac muscle tissue.
- Acid and Alkaline Phosphatases: These enzymes are commonly stained to assess various cellular activities and pathological conditions.
BASIC MICROSCOPY
Introduction:
Microscopy is the cornerstone of pathology, akin to the stethoscope for physicians and the speculum for gynecologists. It enables pathologists to visualize and analyze minute structures and is indispensable for diagnosing diseases.
Types of Microscopes:
- Simple Microscope:
- A basic hand magnifying lens with magnification ranging from 2x to 200x.
- Used for low-magnification observation of larger specimens.
- Compound Microscope:
- Consists of a complex instrument with a series of lenses.
- Objective lens near the specimen and an eyepiece lens near the observer’s eye.
- Offers higher magnification and resolution compared to a simple microscope.
- Can be monocular (single eyepiece) or binocular (two eyepieces), with binocular microscopes being more common.
- Multi-headed microscopes are utilized for teaching and demonstration purposes.
Variants of Light Microscopy:
- Dark Ground Illumination (DGI):
- Used for observing unstained living microorganisms like Treponema pallidum.
- Microorganisms are illuminated by an oblique ray of light, which doesn’t pass through them directly.
- The condenser is blackened in the center, allowing light to pass through its periphery and illuminate the microorganism on a glass slide.
- Polarising Microscope:
- Employed for demonstrating birefringence in substances like amyloid or foreign bodies.
- Light is made plane-polarized, with rays vibrating in a single plane at right angles to each other.
- Two prism discs, known as the polarizer and analyzer, are placed in the light path.
- The lower disc (polarizer) is rotated to ensure light becomes plane-polarized before passing through the specimen.
IMMUNOFLUORESCENCE
Introduction:
The immunofluorescence technique revolutionizes pathology by providing a robust method to visualize and analyze antigenic molecules within cellular structures. This technique relies on the specific binding of antibodies to target antigens, coupled with the detection of fluorescent signals under a microscope, enabling precise localization and identification of cellular components.
Key Components:
- Fluorescence Microscope:
- Utilizes ultraviolet or blue light to excite fluorochromes conjugated to antibodies, causing them to emit light at a longer wavelength.
- Sophisticated systems incorporate filters and condensers to control excitation and emission wavelengths, enhancing signal-to-noise ratio and visualization.
- Techniques:
- Direct Immunofluorescence (IF): Involves the direct conjugation of fluorochromes to primary antibodies, facilitating the visualization of antigen-antibody complexes. While straightforward, it may lack sensitivity due to potential steric hindrance.
- Indirect Immunofluorescence: This versatile approach employs primary antibodies specific to target antigens, followed by the addition of secondary antibodies conjugated to fluorochromes. Indirect IF amplifies signal intensity and allows for signal amplification through multiple secondary antibodies binding to a single primary antibody.
Applications:
- Autoantibody Detection:
- Immunofluorescence aids in the detection of autoantibodies present in patient serum, including antinuclear antibodies (ANA), anti-double-stranded DNA (anti-dsDNA), and anti-cyclic citrullinated peptide (anti-CCP) antibodies. These biomarkers play pivotal roles in diagnosing autoimmune diseases such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA).
- Renal Pathology:
- Immunofluorescence is indispensable for characterizing renal diseases by detecting immune complex deposition within glomeruli. It assists in diagnosing various glomerulonephritis subtypes, including lupus nephritis, membranous nephropathy, and IgA nephropathy.
- Dermatopathology:
- In dermatology, immunofluorescence identifies immune deposits along the dermo-epidermal junction, aiding in the diagnosis of autoimmune blistering disorders like pemphigus vulgaris and bullous pemphigoid.
- Infectious Disease Diagnostics:
- Immunofluorescence enables the detection of viral antigens in infected tissues, facilitating the diagnosis of viral infections such as influenza, herpes simplex virus (HSV), and cytomegalovirus (CMV). Additionally, it plays a crucial role in identifying bacterial pathogens in clinical specimens.
- Research Applications:
- Beyond diagnostics, immunofluorescence serves as a valuable tool for research, enabling the study of cellular signaling pathways, protein localization, and cell-cell interactions in both normal and disease states.
ELECTRON MICROSCOPY
Introduction:
Electron microscopy (EM), pioneered in the 1930s, has revolutionized our understanding of cellular structures and functions by offering unprecedented resolution at the level of cell organelles. While the widespread adoption of diagnostic immunohistochemistry in pathology has somewhat limited its clinical use, EM remains indispensable in specific diagnostic and research settings.
Key Applications:
- Renal Pathology:
- EM, in conjunction with light microscopy and immunofluorescence, plays a crucial role in elucidating the ultrastructural features of renal diseases, aiding in the diagnosis and classification of glomerular disorders.
- Tumors of Uncertain Histogenesis:
- EM helps characterize tumors with ambiguous histology by revealing distinctive ultrastructural features, facilitating their classification and providing insights into their cellular origin and behavior.
- Subcellular Studies in Storage Diseases:
- EM allows for detailed examination of cellular components, particularly in storage diseases where abnormal accumulations of substances within organelles can be visualized, aiding in diagnosis and research.
- Research Purposes:
- EM remains invaluable for basic research, enabling scientists to explore cellular ultrastructure, investigate disease mechanisms, and develop novel therapeutic strategies.
Types of Electron Microscopy:
- Transmission Electron Microscope (TEM):
- TEM is the preferred tool for studying cellular ultrastructure at the organelle level. It involves passing a beam of electrons through ultrathin tissue sections, providing high-resolution images with magnifications ranging from 2,000 to 10,000 times.
- Scanning Electron Microscope (SEM):
- SEM offers a three-dimensional visualization of cell surface architecture, making it suitable for studying intricate surface features such as podocytes in renal glomeruli.
Technical Considerations:
- Fixation:
- Tissue specimens for EM examination are fixed in buffered glutaraldehyde or a formalin-glutaraldehyde mixture, followed by post-fixation in osmium tetroxide to enhance contrast.
- Embedding:
- Specimens are embedded in plastic resin on grids to provide structural support for sectioning.
- Sectioning:
- Semithin sections (1 μm thick) stained with methylene blue or toluidine blue are initially cut to guide subsequent ultrathin sectioning. Ultrathin sections are then obtained using a diamond knife for detailed ultrastructural analysis.
- Staining:
- Thin sections may be stained with lead citrate and uranyl acetate to enhance electron density and improve contrast for better visualization under the electron microscope.
IMMUNOHISTOCHEMISTRY
Introduction:
Immunohistochemistry (IHC) is a pivotal technique in cellular pathology, facilitating the detection and localization of specific antigens within cells using antibodies. By visualizing these antigens as brown coloration, IHC aids in identifying cell lineage and confirming infections, thereby enhancing diagnostic precision and clinical decision-making.
Evolution and Impact:
IHC represents a paradigm shift in diagnostic pathology, often referred to as the “brown revolution,” as it has supplanted histochemistry in many advanced laboratories. Its objective, specific, and reproducible results have transformed surgical pathology, reducing inter-observer variability and adding objectivity to diagnoses. From its early roots in immunofluorescence methods to its current widespread use in formalin-fixed paraffin-embedded tissue blocks, the evolution of IHC has profoundly impacted diagnostic surgical pathology, enhancing its reliability and clinical utility.
Principles and Techniques:
IHC employs antibodies labeled with enzymes, such as horseradish peroxidase, to bind specific antigens in tissue sections. These antibodies form immune complexes with target antigens, which are then visualized using chromogens like diaminobenzidine tetrahydrochloride (DAB) and aminoethyl carbazole (AEC), producing stable brown coloration. Two common methods are the peroxidase-antiperoxidase (PAP) and avidin-biotin conjugate (ABC) techniques, known for their robust staining and specificity.
Antibody Selection:
Choosing antibodies for IHC staining involves careful consideration of the differential diagnosis observed on hematoxylin and eosin (H&E) stained sections. Panels of antibodies, rather than single tests, are preferred to enhance diagnostic accuracy. Antibodies can be polyclonal or monoclonal, with the latter providing high-affinity specificity. Positive controls, such as tissues expressing the target antigen, ensure assay reliability and validate staining quality.
Applications:
- Tumors of Uncertain Histogenesis:
- IHC plays a pivotal role in resolving diagnostic challenges posed by tumors with ambiguous origins, aiding in distinguishing primary from metastatic lesions. Antibody panels targeting intermediate filaments and other markers contribute significantly to accurate diagnosis and treatment planning.
- Prognostic Markers in Cancer:
- IHC serves as a valuable tool in predicting tumor prognosis by detecting micrometastases and identifying molecular markers associated with aggressive behavior. Markers such as HER-2/neu, p53, and Ki67 offer valuable insights into tumor biology, guiding treatment decisions and improving patient outcomes.
- Prediction of Therapy Response:
- IHC assists in predicting therapeutic response in hormone-sensitive cancers like breast and prostate carcinoma. Assessment of receptor expression levels (e.g., estrogen and androgen receptors) guides hormone therapy decisions, leading to more personalized and effective treatment strategies.
- Infectious Diseases:
- IHC confirms tissue infections by detecting microbial antigens using specific antibodies against viral, bacterial, and parasitic agents. This aids in the diagnosis of infectious diseases such as hepatitis, cytomegalovirus infection, and Helicobacter pylori-associated gastritis, facilitating appropriate treatment interventions.
CYTOGENETICS
Introduction:
Karyotyping is a fundamental technique in cytogenetics, involving the systematic arrangement of chromosomes to detect chromosomal abnormalities and genetic disorders. Here, we outline the technical process involved in karyotyping and its applications in diagnostic pathology.
Human Chromosome Composition:
Human somatic cells are diploid, containing 46 chromosomes: 22 pairs of autosomes and one pair of sex chromosomes (XX in females, XY in males). Gametes, or haploid cells, contain 23 chromosomes, with ova carrying 23X and sperms containing either 23X or 23Y chromosomes, determining the offspring’s sex based on paternal chromosomal contribution.
Procedure:
- Cell Selection:
- Cells capable of growth and division, such as those from amniotic fluid, chorionic villus sampling, peripheral blood lymphocytes, bone marrow, and solid tumors, are selected for analysis.
- Cell Culture:
- The obtained sample is cultured in mitogen media, substances inducing cell division (mitosis), like PPD, PHA, PWM, or phorbol ester. Colchicine or colcemid is added to arrest cells in metaphase, followed by lysing in a hypotonic solution. Metaphase cells are fixed in methanol-glacial acetic acid mixture.
- Staining/Banding:
- Chromosomes exhibit alternating dark and light bands when stained. Techniques include:
- Giemsa banding (G-banding): Most common method.
- Quinacrine banding (Q-banding): Demonstrates bands along chromosomes.
- Constitutive banding (C-banding): Highlights constitutive heterochromatin.
- Reverse staining Giemsa banding (R-banding): Yields patterns opposite to G-banding.
- Chromosomes exhibit alternating dark and light bands when stained. Techniques include:
- Microscopic Analysis:
- Chromosomes are photographed, examined under a microscope, and cut. They are then arranged based on size, centromere position, and banding patterns. Chromosome pairs are identified by arm length, with the centromere dividing each chromosome into a short (p) and a long (q) arm.
Applications:
- Chromosomal Numerical Abnormalities:
- E.g., Down’s syndrome (trisomy 21), Klinefelter’s syndrome (XXY), Turner’s syndrome (XO), and spontaneous abortions.
- Chromosome Structural Abnormalities:
- E.g., translocations (e.g., Philadelphia chromosome), cri-du-chat syndrome (5p deletion), deletions, insertions, isochromosomes, and ring chromosome formation.
- Cancer Diagnosis:
- Detects chromosomal abnormalities associated with leukemia, lymphoma, germ cell tumors, and certain sarcomas, aiding diagnosis and prognosis.
DIAGNOSTIC MOLECULAR PATHOLOGY
Introduction
In the last quarter of the 20th century, significant progress in molecular biology has led to the development of molecular techniques for diagnostic purposes, enabling the detection of abnormalities at the DNA or RNA level. These techniques employ hybridization, wherein a labeled probe binds to a specific region of DNA or RNA. Here’s an overview of some molecular methods used in diagnostic pathology:
1. In Situ Hybridization (ISH):
- Principle: ISH allows the localization of nucleic acid sequences directly within intact cells without DNA extraction. A labeled nucleic acid probe hybridizes specifically to its complementary target DNA or RNA in the tissue.
- Applications:
- Detection of viral infections (e.g., HPV, EBV, HIV).
- Gene expression analysis and oncogene detection in human tumors.
- Identification of chromosomal disorders, particularly using fluorescent in situ hybridization (FISH).
2. Filter Hybridization:
- Principle: Target DNA or RNA is extracted from the tissue and immobilized on a filter (nitrocellulose or nylon). Hybridization with a labeled probe is then performed.
- Methods:
- Slot and dot blots: Direct binding of DNA sample to the filter.
- Southern blot: DNA size fractionation by gel electrophoresis prior to hybridization.
- Northern blot: Similar to Southern blot but for RNA size fractionation.
- Applications:
- Neoplasia diagnosis (hematologic and non-hematologic).
- Infectious disease diagnosis and epidemiologic studies.
- Diagnosis of inherited genetic diseases, carrier testing, and prenatal diagnosis.
- Identity determination in tissue transplantation, forensic pathology, and parentage testing.
3. Polymerase Chain Reaction (PCR):
- Principle: PCR amplifies a specific DNA sequence exponentially using DNA polymerase and short complementary DNA fragments (primers). The process involves cycles of denaturation, annealing, and extension.
- Applications:
- Similar to filter hybridization techniques but with advantages such as rapidity, automation with thermal cyclers, and requiring a lower amount of starting DNA.
- Widely used in diagnostics and research for neoplasia, infectious diseases, and inherited genetic diseases.
- Considerations: PCR requires extreme caution to prevent contamination due to its sensitivity.
OTHER MODERN AIDS IN
DIAGNOSTIC PATHOLOGY
1. Flow Cytometry:
- Principle: Flow cytometry analyzes properties of cells suspended in a single moving stream, overcoming subjectivity in microscopic examination. It employs laser-light sources, fluorescence, and computer analysis.
- Applications: Used for immunophenotyping of hematopoietic neoplasms, measuring proliferation-associated antigens, nucleic acid content, diagnosing immunodeficiency, and identifying allograft rejection in transplantation.
2. Methods for Cell Proliferation Analysis:
- Mitotic Count: Counts mitotic cells per high-power field.
- Radioautography: Labels proliferating cells with thymidine and counts labeled cells per 2000 tumor cell nuclei.
- Microspectrophotometric Analysis: Measures DNA content stained with Feulgen reaction.
- Immunohistochemistry: Counts positive cells for proliferation markers like Ki-67, PCNA, and cyclins.
- Nucleolar Organizer Region (NOR) Staining: Identifies nucleolar regions by silver staining.
3. Computers in Pathology Laboratory:
- Purpose: Used for billing, result reporting, data storage, retrieval, and research purposes.
- Advantages: Improves patient care, shortens turnaround time, enhances productivity, enables coding and indexing of results, mandatory for research grants.
4. Speech Recognition System:
- Transforms spoken descriptions into text for gross and microscopic reports without secretarial staff.
5. Image Analyzer and Morphometry:
- Purpose: Provides objective measurement of microscopic features using a system comprising a microscope, computer, image capture board, and analysis software.
- Applications: Morphometric study of tumor cells, nuclear DNA ploidy measurement, quantitative evaluation of immunohistochemical staining.
6. DNA Microarrays:
- Utilizes silicon chip technology for simultaneous analysis of large data volumes related to human genes, aiding molecular profiling of tumors for histogenetic diagnosis and prognosis prediction.
7. Laser Microdissection:
- Involves dissection of single cells or parts using laser technology for molecular profiling on tissue material.
8. Telepathology and Virtual Microscopy:
- Telepathology: Enables diagnostic pathology remotely using transmitted tissue specimen images.
- Virtual Microscopy: Involves high-speed scanners to prepare virtual pathology slides stored in computers for examination and reporting, holding potential for pathology education and clinical meetings.