Red bone marrow is a fascinating and essential tissue that plays a pivotal role in the human body. Understanding its histological structure and function is critical for medical students, as it forms the foundation for many clinical concepts, including hematopoiesis, immune response, and bone marrow-related diseases. This article will explore the histology, structure, and function of red bone marrow, with insights into its clinical relevance, using simple yet informative language.
Table of Contents
What is Red Bone Marrow?
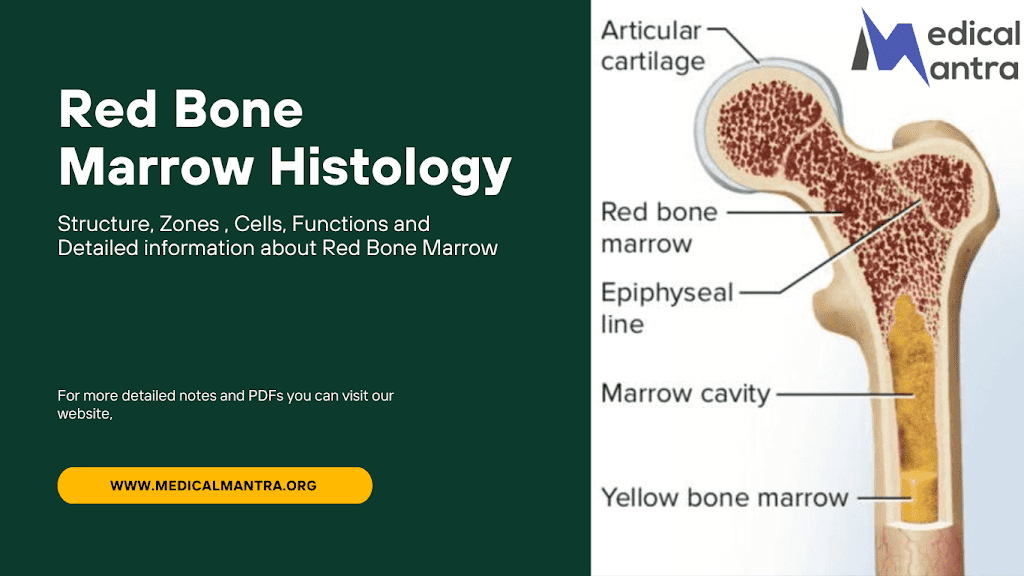
Red bone marrow is a highly specialized, soft, and vascular tissue found within the cavities of certain bones. Unlike yellow bone marrow, which primarily stores fat, red bone marrow is responsible for producing blood cells—a process known as hematopoiesis. It contains an intricate microenvironment that supports the growth and maturation of blood cell precursors. In adults, red bone marrow is predominantly located in flat and irregular bones, such as the pelvis, sternum, ribs, and vertebrae.
Histology of Red Bone Marrow
From a histological perspective, red bone marrow is an organized yet dynamic tissue comprising:
1. Stroma
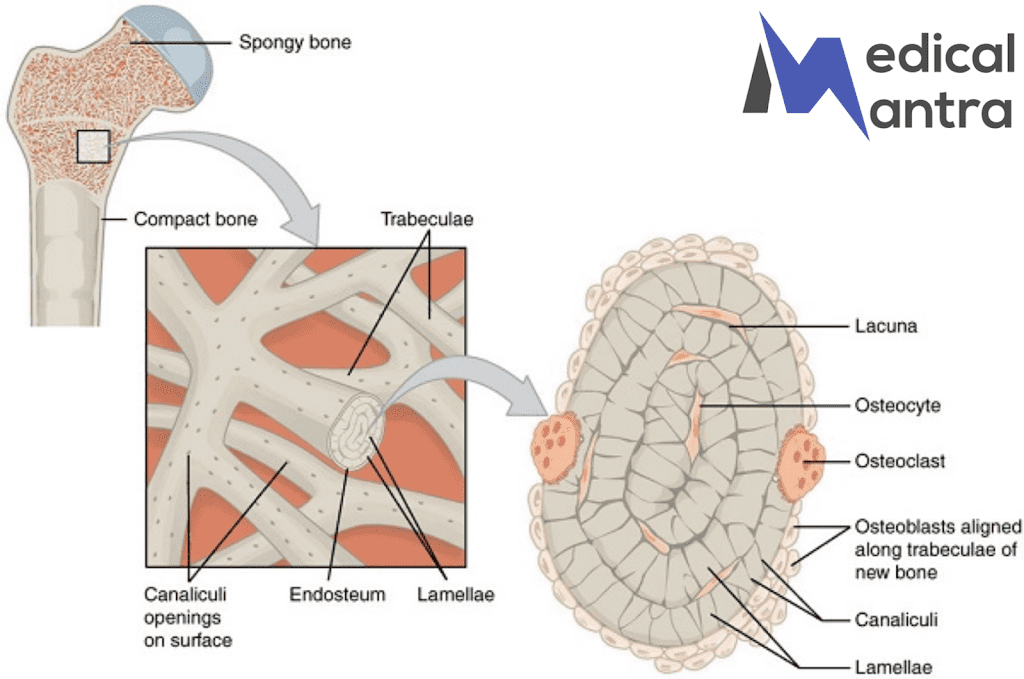
- The stroma forms the supportive framework of red bone marrow, composed of reticular connective tissue. Reticular cells produce a network of reticular fibers that provide structural support.
- The stroma also contains:
- Adipocytes: Fat-storing cells that contribute to the regulation of the hematopoietic environment.
- Fibroblasts: Cells that secrete components of the extracellular matrix.
- Macrophages: Essential for recycling iron from old red blood cells.
2. Hematopoietic Cords
- These are clusters of developing blood cells, including:
- Erythroblasts: Precursors to red blood cells, forming erythroblastic islands.
- Myeloblasts: Precursors to white blood cells like neutrophils and eosinophils.
- Megakaryocytes: Large cells that fragment to form platelets.
3. Sinusoids
- Sinusoids are specialized blood vessels within red bone marrow. They have thin walls and a discontinuous basal lamina, allowing mature blood cells to enter the bloodstream efficiently. These vessels are lined by endothelial cells and supported by adventitial reticular cells.
Functions of Red Bone Marrow
1. Hematopoiesis
Red bone marrow is the primary site of blood cell production, generating:
- Erythrocytes: Red blood cells that transport oxygen.
- Leukocytes: White blood cells that defend against pathogens.
- Thrombocytes: Platelets essential for blood clotting. This process is regulated by growth factors such as erythropoietin and colony-stimulating factors.
2. Immune System Support
Red bone marrow produces B lymphocytes and provides an environment for their maturation. It also contributes to the development of natural killer cells.
3. Iron Recycling
Macrophages in the marrow recycle iron from senescent red blood cells for use in new hemoglobin synthesis, ensuring efficient utilization of this essential mineral.
Differences Between Red and Yellow Bone Marrow
| Feature | Red Bone Marrow | Yellow Bone Marrow |
|---|---|---|
| Primary Function | Hematopoiesis | Fat storage |
| Location (Adults) | Flat and irregular bones | Long bones (diaphysis) |
| Histological Features | Rich in hematopoietic cells and sinusoids | Rich in adipocytes |
| Color | Reddish due to high vascularity | Yellow due to fat content |
Clinical Relevance of Red Bone Marrow
1. Bone Marrow Aspiration and Biopsy
- These procedures are commonly performed to diagnose conditions like leukemia, anemia, and bone marrow infections. Samples are often taken from the iliac crest.
2. Bone Marrow Disorders
- Aplastic Anemia: Failure of bone marrow to produce blood cells.
- Leukemia: Cancer of blood-forming tissues leading to abnormal white blood cell proliferation.
- Myelofibrosis: Scarring of bone marrow, impairing its function.
3. Bone Marrow Transplantation
- In conditions such as leukemia, a bone marrow transplant can replace diseased or damaged marrow with healthy donor marrow, restoring hematopoiesis.
4. Role in Aging and Disease
- With aging, red bone marrow is gradually replaced by yellow marrow in most bones. However, in conditions like chronic anemia, yellow marrow can revert to red marrow to meet increased hematopoietic demand.
Extra Points:-
- Stem Cells: These are the “master builders” of the blood cell world. They start as pluripotential hemopoietic stem cells (PHSCs) and makeup only a tiny fraction of bone marrow cells. They can become various types of blood cells through cell division, including two types of multipotential hemopoietic stem cells (MHSCs) known as CFU-Ly (common lymphoid progenitors) and CFU-GEMM (common myeloid progenitors). Stem cells are like the architects, planning the construction of different blood cell types.
- Progenitor Cells: Progenitor cells are like specialized workers in the bone marrow factory. They’ve chosen their career path and are committed to forming a specific type of blood cell, like eosinophils or lymphoid cells. Hemopoietic factors control their growth and development, and they have limited capacity for self-renewal. These cells are similar in appearance to small lymphocytes.
- Precursor Cells: These cells are the first step in creating mature blood cells. They come from progenitor cells and can’t renew themselves. As they mature, they become smaller, lose their nucleoli, and their cell characteristics start resembling those of the mature blood cells they will eventually become.